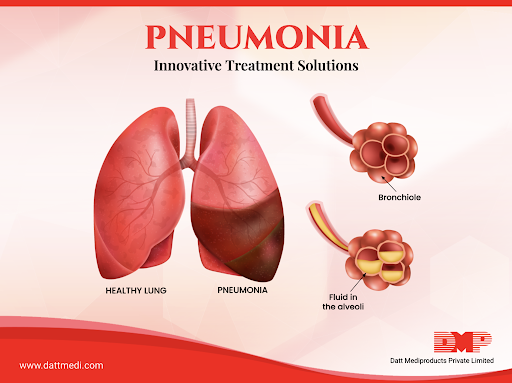
Pneumonia is an inflammatory lung condition that primarily affects the tiny air sacs in the lungs called alveoli. It can be caused by various infectious agents,includig bacteria, viruses, fungi, or other microorganisms.
Overview :
Pneumonia is a common respiratory illness that can affect people of all ages. It can occur as a result of infection, aspiration of foreign substances, or chemical irritants. The most common cause of pneumonia is infection with bacteria or viruses., and it leads to the air sacs filling with pus or other fluids, making it difficult to breathe. Pneumonia can range from mild to severe and can be life-threatening, especially in vulnerable populations.
Difference Between Viral and Bacterial Pneumonia:
- Bacterial Pneumonia: This type of pneumonia is caused by bacteria such as Streptococcus pneumoniae or Mycoplasma pneumoniae. It often comes on suddenly and can be more severe. Symptoms may include high fever, productive cough with thick mucus, and chest pain.
- Viral Pneumonia: Viral pneumonia is caused by viruses like influenza, respiratory syncytial virus (RSV), or COVID-19. It usually has a more gradual onset and may be less severe than bacterial pneumonia. Symptoms often include fever, dry cough, and fatigue.
Types of Pneumonia:
There are several types of pneumonia, including:
1.Community-Acquired Pneumonia (CAP):
- Definition: CAP is acquired outside of healthcare facilities and is typically caused by bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, or Mycoplasma pneumoniae.
- Diagnosis: Diagnosis involves a physical examination, medical history, and diagnostic tests. Chest X-rays, blood tests (such as complete blood count), and sputum cultures are common diagnostic tools.
- Treatment: Treatment usually consists of antibiotics, with the choice of antibiotic depending on the suspected or identified causative agent. The choice of antibiotics may be guided by local antibiotic resistance patterns.
- Hospital-Acquired Pneumonia (HAP):
- Definition: HAP occurs during a hospital stay and is often associated with healthcare procedures and equipment. It can be caused by a range of bacteria, including drug-resistant strains.
- Diagnosis: Similar to CAP, diagnosis includes physical examination and diagnostic tests. Chest X-rays and blood cultures are essential for diagnosing HAP.
- Treatment: Treatment may require broad-spectrum antibiotics initially, pending the results of cultures and sensitivity tests. Antibiotic choice may need to be adjusted based on culture results and the patient’s clinical response. Prevention is key through infection control measures.
- Ventilator-Associated Pneumonia (VAP):
- Definition: VAP occurs in patients who are on mechanical ventilation. It often results from the aspiration of bacteria from the oropharynx into the lungs.
- Diagnosis: Diagnosis is challenging because patients on ventilators may not exhibit typical symptoms. Chest X-rays, blood cultures, and bronchoalveolar lavage (BAL) samples are used for diagnosis.
- Treatment: Treatment includes antibiotics effective against common VAP pathogens, such as Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus (MRSA). Prevention measures, including strict infection control, are crucial.
- Aspiration Pneumonia:
- Definition: Aspiration pneumonia results from the inhalation of foreign substances, typically gastric contents or food particles, into the lungs. This can lead to inflammation and infection.
- Diagnosis: Diagnosis is based on clinical history, physical examination, and imaging studies like chest X-rays. Confirmation may require analysis of respiratory secretions.
- Treatment: Treatment involves addressing the underlying cause of aspiration, such as correcting swallowing difficulties or removing obstructing objects. Antibiotics may be necessary if infection is present.
- Atypical Pneumonia:
- Definition: Atypical pneumonia is often caused by atypical bacteria like Mycoplasma pneumoniae, Chlamydia pneumoniae, or Legionella pneumophila, as well as some viruses.
- Diagnosis: Diagnosis relies on clinical symptoms, physical examination, and specific laboratory tests like serology or PCR for atypical pathogens.
- Treatment: Antibiotics such as macrolides or tetracyclines are typically used to treat a typical pneumonia caused by bacteria. Viral atypical pneumonia is managed symptomatically and may require antiviral medications if available.
Sign and Symptoms:
Bacterial Pneumonia Symptoms:
- High fever
- productive cough with yellow or green mucus
- chest pain
- rapid breathing, and confusion in older adults
Viral Pneumonia Symptoms:
- fever
- dry cough
- muscle aches
- fatigue, and shortness of breath

Causes of pneumonia:
Pneumonia can be caused by various factors, but the most common are infectious agents such as bacteria, viruses, or fungi. In some cases, non-infectious factors like chemical irritants or aspiration of foreign substances can also lead to pneumonia.
Infectious Causes of Pneumonia:
- Bacterial Pneumonia:
- Streptococcus pneumoniae (Pneumococcus): This is the most common bacterial cause of pneumonia. It often occurs as a complication of upper respiratory tract infections.
- Haemophilus influenzae: Particularly type b (Hib), this bacterium can cause pneumonia, especially in young children.
- Mycoplasma pneumoniae: This bacterium causes atypical or “walking” pneumonia, which is generally milder than typical bacterial pneumonia.
- Legionella pneumophila: Responsible for Legionnaires’ disease, it can lead to severe pneumonia, especially in individuals with weakened immune systems.
- Staphylococcus aureus: Can cause both community-acquired pneumonia and healthcare-associated pneumonia, sometimes with severe symptoms.
- Klebsiella pneumoniae: Common in older adults and individuals with certain risk factors like alcoholism or chronic lung disease, it can cause severe pneumonia.
- Viral Pneumonia:
- Influenza viruses (Flu): Seasonal influenza strains can lead to viral pneumonia, which can be severe, especially in young children, the elderly, and those with underlying health conditions.
- Respiratory syncytial virus (RSV): Primarily affects infants and young children, causing bronchiolitis and pneumonia.
- Adenoviruses: Can cause pneumonia, especially in military recruits and crowded living conditions.
- Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2): The virus responsible for COVID-19 can lead to viral pneumonia in some cases, which can be severe and life-threatening.
- Fungal Pneumonia:
- Pneumocystis jirovecii: Common in individuals with weakened immune systems, such as those with HIV/AIDS, this fungus can cause a type of pneumonia called Pneumocystis pneumonia (PCP).
- Candida, Aspergillus, and other fungi: These can cause pneumonia, particularly in immunocompromised individuals or those with pre-existing lung conditions.
- Other Pathogens:
- Tuberculosis (Mycobacterium tuberculosis): Tuberculosis can affect the lungs, causing a type of pneumonia known as tuberculous pneumonia.
- Atypical Bacteria: Other bacteria like Chlamydophila pneumoniae and Coxiella burnetii can cause atypical pneumonia.
Non-Infectious Causes of Pneumonia:
While infections are the most common causes of pneumonia, non-infectious factors can also contribute, including:
- Aspiration: Inhaling food, liquids, or other foreign substances into the lungs can lead to chemical or aspiration pneumonia.
- Chemical irritants: Inhaling toxic chemicals or gases can damage lung tissue and cause pneumonia.
- Physical injury: Chest trauma or inhalation of smoke or burn injuries can result in pneumonia.
- Autoimmune diseases: Conditions like lupus or rheumatoid arthritis can cause inflammation in the lungs, leading to pneumonia.
Prevention:
Preventive measures include vaccination against common bacterial and viral causes of pneumonia (e.g., pneumococcal and influenza vaccines), good hygiene practices, and avoiding smoking and excessive alcohol consumption.
Is Pneumonia Contagious?
Yes, pneumonia is contagious, especially if it is caused by infectious agents like bacteria or viruses. It can spread through respiratory droplets when an infected person coughs or sneezes. It’s essential to practice good respiratory hygiene, such as covering your mouth and nose when coughing or sneezing, to reduce the risk of spreading pneumonia to others. Viral pneumonia, like COVID-19, can be highly contagious. Bacterial pneumonia is less contagious but can still spread to close contacts. Prompt treatment with antibiotics or antiviral drugs can help reduce contagiousness.
Diagnosis:
- Physical Examination: Doctors assess vital signs, listen to lung sounds, and check for symptoms such as cough, fever, and breathing difficulties.
- Imaging: Chest X-rays or CT scans can reveal infiltrates or areas of consolidation in the lungs.
- Laboratory Tests: Blood tests, sputum cultures, and blood cultures may be performed to identify the causative agent and its susceptibility to antibiotics.
- Bronchoscopy: In some cases, a bronchoscopy may be necessary to collect samples from the lungs for culture or analysis.
Management and Treatment:
- Antibiotics: Bacterial pneumonia is typically treated with antibiotics. The choice of antibiotic depends on the type of pneumonia, the patient’s age and health, and local resistance patterns.
- Antiviral Medications: Viral pneumonia, such as influenza or COVID-19, may require antiviral drugs if available and indicated.
- Supportive Care: This includes rest, hydration, and over-the-counter medications to relieve symptoms like fever and cough.
- Oxygen Therapy: In severe cases with low oxygen levels, supplemental oxygen may be provided.
- Hospitalization: Some cases, especially in the elderly or immunocompromised individuals, may require hospitalization for close monitoring and intravenous antibiotics.
The specific diagnosis and treatment plan for pneumonia will be determined by the patient’s clinical presentation and the causative agent identified through diagnostic tests. Early diagnosis and appropriate treatment are essential for a better prognosis and reducing the risk of complications.

Dr. Hamza is a medical content reviewer with over 12 years of experience in healthcare research and patient education. He specializes in evidence-based health information, medications, and chronic disease management. His reviews are based on trusted medical sources and current clinical guidelines to ensure accuracy, transparency, and reliability. All content reviewed by Dr. Hamza is intended for educational purposes only and should not be considered a substitute for professional medical advice










Great content! Super high-quality! Keep it up!
May I request more information on the subject? All of your articles are extremely useful to me. Thank you!
Sustain the excellent work and producing in the group!
You’ve the most impressive websites.
Can you write more about it? Your articles are always helpful to me. Thank you!
Thanks for your help and for writing this post. It’s been great.