Generic name: Ketoconazole
Brand names: Nizoral, Xolegel, Ketodan
Drug class: anti-fungal
Ketoconazole is an antifungal medication that belongs to the azole class of drugs.Ketoconazole used to treat various fungal infections, including those caused by Candida species and dermatophytes. Ketoconazole was first introduced in the late 1970s. It was initially developed as an oral antifungal agent for systemic infections. Over time, ketoconazole has been used both topically and systemically to treat various fungal infections.
Pharmacology
How does ketoconazole work?
Ketoconazole inhibits the synthesis of ergosterol, a key component of fungal cell membranes, by blocking the activity of the enzyme lanosterol 14-alpha-demethylase. This disruption impairs the integrity of the fungal cell membrane,leading to cell death.
Spectrum of Activity: Ketoconazole is effective against a broad range of fungi,including Candida species and dermatophytes.
Pharmacokinetics:
● Absorption: Ketoconazole is absorbed well from the gastrointestinal tract but may be influenced by factors such as food and gastric acidity.
● Distribution: It is widely bound to plasma proteins.
● Metabolism: Ketoconazole undergoes hepatic metabolism, primarily through the cytochrome P450 system, specifically the CYP3A4 enzyme.
● Excretion: The drug and its metabolites are excreted in the urine and bile.
Onset of Action: The onset of antifungal activity is gradual, and therapeutic effects may take several days to become apparent.
Duration of Action: The duration of action is typically prolonged, allowing for less frequent dosing in some cases.
Dosage form of ketoconazole:
Ketoconazole is available in several dosage forms, including oral tablets, topical creams, shampoos, and foam. Each form is designed to target different types of fungal infections and provide effective treatment.
Oral Tablets:
Ketoconazole is commonly formulated as oral tablets. These tablets are usually white or off-white, and their appearance may vary depending on the manufacturer.
Strengths: Oral ketoconazole tablets are available in various strengths,commonly ranging from 200 mg per tablet.
Dosage and Administration: The typical dosage for oral ketoconazole varies depending on the type and severity of the fungal infection. It is usually taken with a meal to enhance absorption.
Topical Creams:
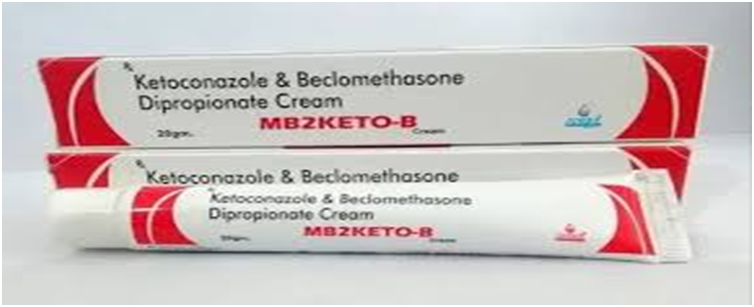
Ketoconazole topical creams are designed for external use on the skin. They are often white or cream-colored.
Strengths: Creams typically come in various concentrations, commonly 1% or 2% ketoconazole.
Dosage and Administration: Topical creams are applied to the affected skin areas in a thin layer, usually once or twice daily, as directed by a healthcare professional.
Topical Shampoos:
Ketoconazole shampoos are specifically formulated for application to the scalp and hair.
Strengths: Shampoos are commonly available in 1% or 2% concentrations of ketoconazole.
Dosage and Administration: The shampoo is applied to wet hair, massaged into the scalp, and left on for a few minutes before rinsing. Frequency of use may vary based on the specific product and the severity of the condition.

Topical Foam:
Ketoconazole foam is a newer formulation that may offer ease of application and better coverage compared to creams or shampoos.
Strengths: Similar to creams and shampoos, ketoconazole foam is available in various concentrations, typically 2%.
Dosage and Administration: The foam is applied to the affected skin or scalp as directed, usually once daily.
Medical uses on the basis of dosage form:
It’s important to note that the choice of dosage form depends on the type and location of the fungal infection.
1.Oral Tablets:
Systemic Fungal Infections: Oral ketoconazole is primarily indicated for the treatment of systemic fungal infections, including:
● Candidiasis (systemic or mucosal infections caused by Candida species).
● Histoplasmosis (caused by the fungus Histoplasma capsulatum).
● Blastomycosis (caused by the fungus Blastomyces dermatitidis).
● Coccidioidomycosis (caused by the fungus Coccidioides immitis).
- Topical Creams:
Cutaneous fungal infections: ketoconazole cream is used topically for localized fungal infections of the skin, including:
● Tinea infections (ringworm) such as tinea corporis, tinea cruris,
and tinea pedis.
● Cutaneous candidiasis (skin infections caused by Candida
species).
● Seborrheic dermatitis.
- Topical Shampoos:
Scalp Conditions: Ketoconazole shampoos are commonly indicated for conditions affecting the scalp, including:
● Seborrheic dermatitis of the scalp.
● Dandruff caused by the overgrowth of Malassezia, a yeast-like
fungus.
The duration of treatment and frequency of application vary based on the severity of the infection and the specific product prescribed. Systemic infections often require oral administration for the drug to reach the bloodstream and target the infection internally. On the other hand, topical formulations are suitable for
localized infections on the skin or scalp.
What other medicines will affect ketoconazole topical?
Medicine used on the skin isn’t likely to be affected by other medicines you use. Numerous oral medicines can interact with each other.
Side effects of ketoconazole:
Ketoconazole, like any medication, can have side effects. The side effects can vary depending on the dosage form (oral, topical cream, shampoo, etc.)
Common side effects include:
● Nausea
● Vomiting
● Abdominal pain
● Dyspepsia
● flatulence
● Adrenal Insufficiency (rare)
Serious Side Effects:
● Yellowing of eyes/skin (jaundice)
● Persistent nausea or vomiting
● Severe stomach or abdominal pain
● Dark urine
● Severe Skin Reactions
What happens if I overdose?
An overdose of ketoconazole topical isn’t anticipated to be dangerous. Seek urgent medical attention or call the Poison Help Line at 1-800-222-1222 if anyone has accidentally swallowed the drug.
Drug-Drug interaction
It’s essential to consult with a healthcare professional before combining ketoconazole with other medications. Below are some notable drug interactions with ketoconazole:
- CYP3A4 Inhibitors: Ketoconazole is a potent inhibitor of the cytochrome P450 enzyme CYP3A4. Drugs metabolized by CYP3A4 may experience increased levels and prolonged effects when used concomitantly with ketoconazole. This includes medications like:
● Cyclosporine
● Warfarin
● Certain statins (simvastatin, lovastatin)
● Calcium channel blockers (e.g., felodipine, nifedipine)
● Benzodiazepines (e.g., midazolam, triazolam) - QT Prolongation Agents: Ketoconazole has been associated with QT interval prolongation, and combining it with other drugs that also prolong the QT interval may increase the risk of serious arrhythmias. Such drugs include:
● Certain antipsychotics (e.g., haloperidol, thioridazine)
● Class Ia and III antiarrhythmics (e.g., quinidine, amiodarone) - HIV Medications: Ketoconazole may interact with some HIV medications,particularly protease inhibitors. Examples include:
● Ritonavir
● Atazanavir - Hormonal Contraceptives: Ketoconazole may reduce the effectiveness of hormonal contraceptives. Women using oral contraceptives should consider alternative methods of contraception during ketoconazole therapy.
- Corticosteroids: Concurrent use of ketoconazole with certain corticosteroids may increase the risk of adrenal insufficiency.
- Antacids and H2 Blockers: These drugs may reduce the absorption of ketoconazole. It is advisable to take ketoconazole at least 2 hours before or after antacids or H2 blockers.

Contraindications of Ketoconazole:
Ketoconazole has certain contraindications, meaning situations or conditions in which the use of the medication is not recommended due to the potential for harm.
- Hypersensitivity: Individuals who have demonstrated hypersensitivity or allergic reactions to ketoconazole or any of its components should not use this medication.
- Acute or chronic liver disease: ketoconazole is metabolized in the liver, and its use may be associated with hepatotoxicity. Therefore, individuals with acute or chronic liver disease should exercise caution when using ketoconazole.
- Concomitant Use with Certain Drugs: Contraindications may exist when ketoconazole is used in combination with certain drugs, such as:
● Strong CYP3A4 inducers (e.g., rifampin, carbamazepine)
● HMG-CoA reductase inhibitors (statins) that are metabolized by CYP3A4, like simvastatin and lovastatin
Precautions and Warnings
Liver Function Monitoring: Regular monitoring of liver function is typically recommended, especially with prolonged use of oral ketoconazole.
During Pregnancy:. The use of ketoconazole during pregnancy is generally not recommended unless the potential benefits outweigh the potential risks. Ketoconazole is classified as a pregnancy Category C medication by the U.S. Food and Drug Administration (FDA). This means that there may be potential risks to the fetus, but the decision to use the medication during pregnancy is left to the discretion of the healthcare provider based on individual circumstances.

Dr. Hamza is a medical content reviewer with over 12 years of experience in healthcare research and patient education. He specializes in evidence-based health information, medications, and chronic disease management. His reviews are based on trusted medical sources and current clinical guidelines to ensure accuracy, transparency, and reliability. All content reviewed by Dr. Hamza is intended for educational purposes only and should not be considered a substitute for professional medical advice










Thanks for posting. I really enjoyed reading it, especially because it addressed my problem. It helped me a lot and I hope it will help others too.
Can you write more about it? Your articles are always helpful to me. Thank you!