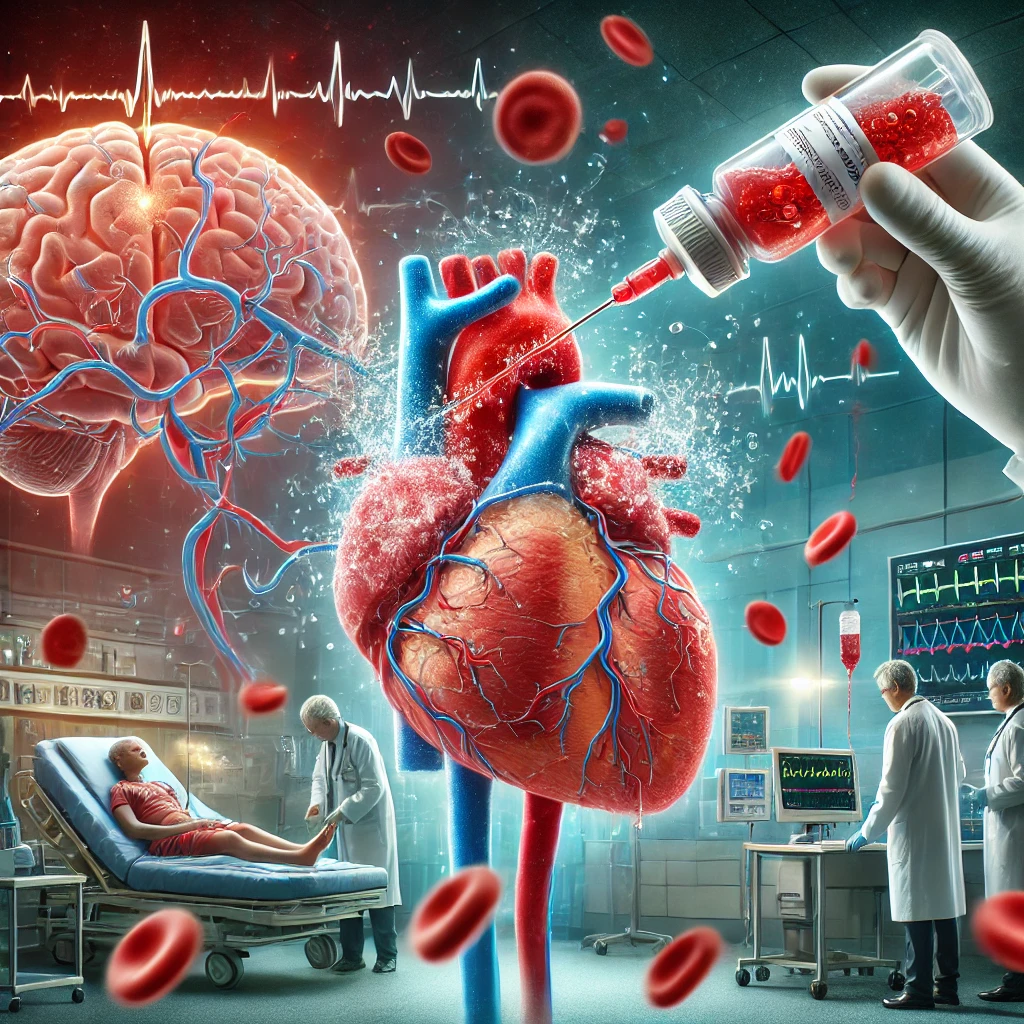
Emergency use of thrombolytic agent in heart attack and stroke dissolves clots fast, restoring blood flow and saving lives. Thrombolytics, also known as fibrinolytic agents or clot busters, are medications used to dissolve blood clots in emergency situations. These drugs play a crucial role in treating life-threatening conditions like heart attacks (myocardial infarction), ischemic strokes, and pulmonary embolism.
What Are Thrombolytics?
Thrombolytics are a class of drugs designed to break down blood clots by activating the body’s natural fibrinolytic system. These medications work by converting plasminogen into plasmin, an enzyme that dissolves fibrin, the structural component of clots.
How does Thrombolytics work?
Emergency use of thrombolytic agents in heart attack and stroke helps dissolve clots, restore blood flow, and improve survival when given promptly.
- Activation of Plasminogen
- Thrombolytics convert plasminogen, an inactive precursor, into plasmin, an active enzyme.
- This conversion is catalyzed by agents like tissue plasminogen activator (tPA) (e.g., alteplase) or streptokinase.
- Fibrin Degradation
- Plasmin breaks down fibrin, the protein mesh that stabilizes a blood clot.
- This process leads to fibrinolysis, effectively dissolving the clot.
- Restoration of Blood Flow
- As the clot dissolves, blood flow resumes in the affected vessel, preventing tissue damage.
- Regulation by Antifibrinolytic Mechanisms
- The body has natural inhibitors like plasminogen activator inhibitor (PAI-1) and α2-antiplasmin, which regulate fibrinolysis to prevent excessive bleeding.
Common thrombolytic agents include:
- Alteplase (tPA) – Frequently used in ischemic strokes and heart attacks.
- Reteplase (rPA) – A recombinant variant used primarily for myocardial infarction.
- Tenecteplase (TNK-tPA) – A genetically modified version with longer half-life and increased specificity.
- Streptokinase – A bacterial-derived enzyme that activates plasminogen.
- Urokinase – Often used for pulmonary embolism and catheter-related thrombosis.
Emergency Uses of Thrombolytics Agent
The emergency use of thrombolytics is critical in situations where blood flow must be restored rapidly to prevent tissue death. Here are the primary conditions where thrombolytics save lives:
1. Emergency Use Of Thrombolytics Agent in Ischemic Stroke
- Time Window: Administered within 3 to 4.5 hours of symptom onset.
- Mechanism: Restores blood flow to the brain by dissolving clots in cerebral arteries.
- Benefit: Reduces disability and improves functional recovery.
2. Emergency Use Of Thrombolytics Agent in Myocardial Infarction (Heart Attack)
- Time Window: Most effective within the first 12 hours.
- Mechanism: Dissolves clots in coronary arteries, restoring blood supply to the heart.
- Benefit: Minimizes heart muscle damage and improves survival rates.
3. Emergency Use Of Thrombolytics Agent in Pulmonary Embolism (PE)
- Time Window: Used in massive PE cases with hemodynamic instability.
- Mechanism: Clears large clots in the lungs to restore oxygenation.
- Benefit: Prevents cardiac arrest and respiratory failure.
4. Emergency Use Of Thrombolytics Agent in Deep Vein Thrombosis (DVT)
- Time Window: Applied in severe DVT cases leading to limb-threatening conditions.
- Mechanism: Dissolves extensive clots in deep veins.
- Benefit: Reduces risk of post-thrombotic syndrome.
5. Emergency Use Of Thrombolytics Agent in Catheter-Related Thrombosis
- Time Window: Used when catheters are blocked due to blood clots.
- Mechanism: Restores patency in central venous catheters.
- Benefit: Maintains access for medical treatments.
Emergency Use Of Thrombolytics Agent: Risks and Contraindications
While thrombolytics are highly effective, they come with potential risks. The major concern is bleeding, which can be life-threatening if not managed properly. Patients with a history of hemorrhagic stroke, recent surgery, or active internal bleeding are typically excluded from thrombolytic therapy. Careful patient selection is essential to maximize benefits while minimizing complications.
Frequently Asked Questions (FAQs)
1. When should thrombolytics be administered in an emergency?
Thrombolytics should be given as soon as possible within the recommended time window for each condition: within 3-4.5 hours for ischemic stroke, within 12 hours for myocardial infarction, and immediately in cases of massive pulmonary embolism.
2. What are the major risks of thrombolytic therapy?
The primary risk is severe bleeding, including intracranial hemorrhage. Other risks include allergic reactions, low blood pressure, and reperfusion arrhythmias.
3. Who should not receive thrombolytics?
Patients with a history of hemorrhagic stroke, recent major surgery, active internal bleeding, or severe hypertension are generally not eligible for thrombolytic therapy.
4. How are thrombolytics administered?
Thrombolytics are typically given via intravenous (IV) infusion in a hospital setting under strict medical supervision.
5. Can thrombolytics be used for all types of strokes?
No, thrombolytics are only used for ischemic strokes caused by blood clots. They are contraindicated in hemorrhagic strokes due to the risk of worsening bleeding.
6. Are there alternatives to thrombolytic therapy?
Yes, mechanical thrombectomy is an alternative for ischemic stroke, and percutaneous coronary intervention (PCI) is preferred for heart attacks when available.