What are antibiotics?
Antibiotics are potent medications designed to kill or inhibit the growth of bacteria. They are not effective against viral infections like the common cold or flu. When used appropriately, antibiotics can save lives by treating bacterial infections and preventing complications. Antibiotics can be derived from natural sources like fungi and bacteria or synthesized in laboratories. Their effectiveness in combating bacterial infections has made them indispensable in modern healthcare. However, their misuse or overuse can lead to antibiotic resistance, posing a significant challenge to global public health.
In today’s fast-paced world, antibiotics play a crucial role in combating bacterial infections. From minor ailments to life-threatening diseases, these medications have revolutionized healthcare.
How do antibiotics work?
Antibiotics are fighter pilots for your body when it comes to bacterial infections. They work in two main ways:
- Killing bacteria: Antibiotics can disrupt essential processes or structures within the bacteria, basically causing them to die. This is like the antibiotic taking out the enemy.
- Stopping growth: Some antibiotics don’t directly kill bacteria, but they make it impossible for them to reproduce. With fewer and fewer bacteria, the immune system can then easily swoop in and clear the infection. This is like the antibiotic stopping the enemy from multiplying its forces.
In which conditions should antibiotics be used?
Antibiotics are commonly used to treat bacterial infections, such as:
- Respiratory infections
- Urinary tract infections
- Skin infections
- Ear infections
- Sexually transmitted infections
- Bacterial meningitis
- Strep throat
- Certain gastrointestinal infections
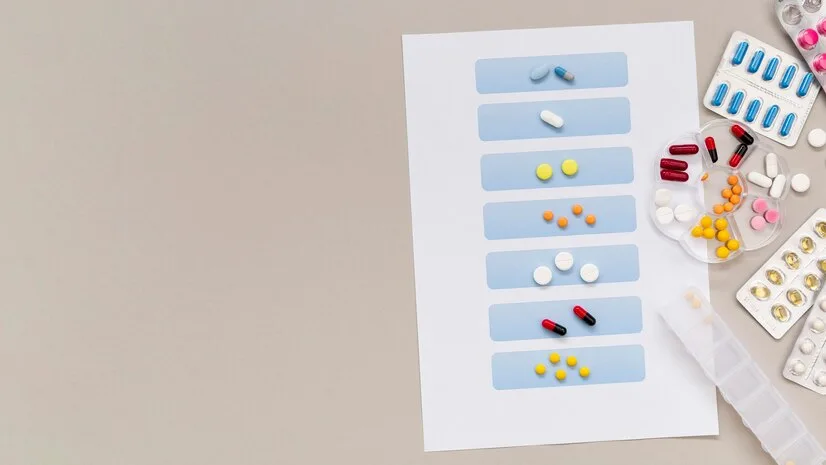
Types of Antibiotics
- Penicillin: Penicillin was the first antibiotic discovered and remains widely used today. It performs their action by interfering with bacterial cell wall synthesis and causing cell death. Examples include amoxicillin and ampicillin.
- Cephalosporins: This class of antibiotics is similar in structure and function to penicillin. They are effective against a broad range of bacteria and are commonly used for respiratory and skin infections. Examples include cephalexin and ceftriaxone .
- Macrolides: Macrolide antibiotics work by inhibiting bacterial protein synthesis. They are often prescribed for respiratory tract infections, such as pneumonia and bronchitis. Examples include azithromycin and clarithromycin.
- Tetracyclines: Tetracycline antibiotics interfere with bacterial protein synthesis and are effective against a wide variety of bacteria. They are used to treat acne, urinary tract infections, and certain sexually transmitted diseases. Examples include doxycycline and minocycline.
- Fluoroquinolones: Fluoroquinolones are broad-spectrum antibiotics that inhibit bacterial DNA synthesis. They are used to treat respiratory, urinary tract, and skin infections. Examples include ciprofloxacin and levofloxacin.
- Aminoglycosides: Aminoglycosides work by disrupting bacterial protein synthesis. They are primarily used to treat severe bacterial infections, particularly those caused by gram-negative bacteria. Examples include gentamicin and amikacin.
- Sulfonamides (Sulfa Drugs): Sulfonamides inhibit bacterial growth by interfering with the synthesis of folic acid, a necessary component for bacterial DNA and RNA synthesis. They are used to treat urinary tract infections, ear infections, and certain types of pneumonia. Examples are sulfamethoxazole-trimethoprim (TMP-SMX).
- Glycopeptides: Glycopeptides target bacterial cell wall synthesis, and causes cell death. They are reserved for treating serious infections caused by gram-positive bacteria, particularly those resistant to other antibiotics. Examples include vancomycin and teicoplanin.
- Oxazolidinones: Oxazolidinones inhibit bacterial protein synthesis by binding to the bacterial ribosome. They are used to treat infections caused by methicillin-resistant Staphylococcus aureus (MRSA) and other multidrug-resistant bacteria. Linezolid is an example of an oxazolidinone antibiotic.
- Lincosamides: Lincosamides work by inhibiting bacterial protein synthesis. They are used to treat various infections, including skin infections, respiratory tract infections, and pelvic inflammatory disease. Clindamycin is a commonly used lincosamide antibiotic.

Side effects of antibiotics:
Common side effect include:
- Diarrhea: Antibiotics can disrupt the balance of good and bad bacteria in your gut, leading to diarrhea.
- Stomach upset: This can include nausea, vomiting, and indigestion.
- Rash: Some people may develop a rash after taking antibiotics.
- Yeast infection: Antibiotics can kill off the fungus that helps keep yeast in check in the body, which can lead to a yeast infection.
- Headache: it is a common difficulty with many medications, including antibiotics.
Irrational use of antibiotics
The irrational use of antibiotics refers to practices that deviate from appropriate and evidence-based guidelines for antibiotic prescribing and usage.
- Overprescribing: prescribing antibiotics when they are not necessary or when a viral infection is the cause. Antibiotics are ineffective against viral infections such as the common cold, flu, and most cases of bronchitis.
- Incomplete Courses: Stopping antibiotic treatment prematurely, before completing the full prescribed course, can contribute to antibiotic resistance. It’s essential to finish the entire course of antibiotics, even if symptoms improve.
- Self-Medication: Taking antibiotics without a prescription or without consulting a healthcare professional can lead to inappropriate use and contribute to antibiotic resistance. Self-medication can also delay the appropriate treatment of bacterial infections and increase the risk of adverse effects.
- Inappropriate Antibiotic Selection: Choosing the wrong antibiotic or using broad-spectrum antibiotics when narrower-spectrum options would suffice can promote antibiotic resistance and disrupt the body’s natural microbiota.
- Prophylactic Use: Using antibiotics prophylactically (preventively) without a clear medical indication can contribute to antibiotic resistance and increase the risk of adverse effects.
Antibiotic resistance
Antibiotic resistance occurs when bacteria develop the ability to withstand the effects of antibiotics, rendering the medications ineffective in killing or controlling bacterial growth. This phenomenon arises primarily through genetic changes in bacteria, either through mutation or the acquisition of resistance genes from other bacteria.
Antibiotic resistance develops when bacteria are exposed to antibiotics, either through overuse, inappropriate use, or incomplete courses of treatment. Antibiotic resistance poses a significant threat to public health, as it limits treatment options for bacterial infections and can lead to prolonged illness, increased healthcare costs, and higher mortality rates.
Conclusion
Antibiotics have revolutionized current medicine and saved countless lives. By using antibiotics responsibly and only when necessary, we can preserve their effectiveness for future generations. Remember, antibiotics are powerful tools in the fight against bacterial infections, but they must be used wisely.
FREQUENTLY ASKED QUESTIONS(FAQ’S)
- Can you buy and take antibiotics by yourself?
No, you should not buy and take antibiotics without consulting a healthcare professional. Self-medication with antibiotics can lead to inappropriate use, antibiotic resistance, and potential adverse effects. Always seek guidance from a healthcare provider before starting any antibiotic treatment.
2. When are antibiotics usually prescribed?
Antibiotics are typically prescribed when there is a bacterial infection diagnosed by a healthcare professional. Common conditions that may warrant antibiotic treatment include bacterial pneumonia, urinary tract infections, skin infections like cellulitis, strep throat, and bacterial sinusitis. It’s essential for antibiotics to be prescribed judiciously based on the type and severity of the infection, as well as other individual factors.
3. How long do you take antibiotics?
The duration of antibiotic treatment depends on several factors, including the type and severity of the infection, the specific antibiotic being used, and individual patient factors. In general, healthcare providers prescribe antibiotics for the shortest effective duration necessary to treat the infection adequately.
For many common bacterial infections, such as urinary tract infections or skin infections, antibiotic courses typically range from 7 to 14 days. However, some infections may require shorter or longer treatment durations.
4. In which conditions should antibiotics not be used?
Antibiotics should not be used in several conditions:
- Viral infections: This is the most common misuse. Antibiotics target bacteria, and viruses are a completely different type of germ. Common illnesses caused by viruses, like the common cold, flu, most coughs, and many sore throats, will not improve with antibiotics and may even lead to unnecessary side effects.
- Self-limiting bacterial infections: Some mild bacterial infections, like some ear infections or uncomplicated sinus infections, can resolve on their own with rest and supportive care. Taking antibiotics in these cases won’t speed up recovery and contributes to resistance.
- Prevention of future infections: Antibiotics are not a preventative measure. They should only be used to treat an existing bacterial infection diagnosed by a doctor.
- When you’re unsure of the cause: If you’re unsure if you have a bacterial or viral infection, consult your doctor. Taking antibiotics unnecessarily increases resistance.
- Someone else’s prescription: Sharing or using leftover antibiotics from someone else’s prescription is dangerous. The medication may not be appropriate for your specific infection, and the dosage could be incorrect.
- Bacterial infections suspected to be resistant: If your doctor suspects a particularly stubborn bacterial infection, they may withhold antibiotics initially to test for specific strains.