Introduction
Amphotericin B is a potent antifungal medication that has been a cornerstone in the treatment of severe fungal infections for decades. Its ability to combat both superficial and systemic mycoses has made it a critical tool in the medical field. However, with great power comes the need for careful management due to its potential side effects and complex administration.
What is Amphotericin B?
Amphotericin B is an antifungal antibiotic derived from the bacterium Streptomyces nodosus. Discovered in the 1950s, it has since become a primary treatment for life-threatening fungal infections, particularly in immunocompromised patients. Chemically, it is a polyene macrolide, known for its broad-spectrum activity against fungal pathogens.
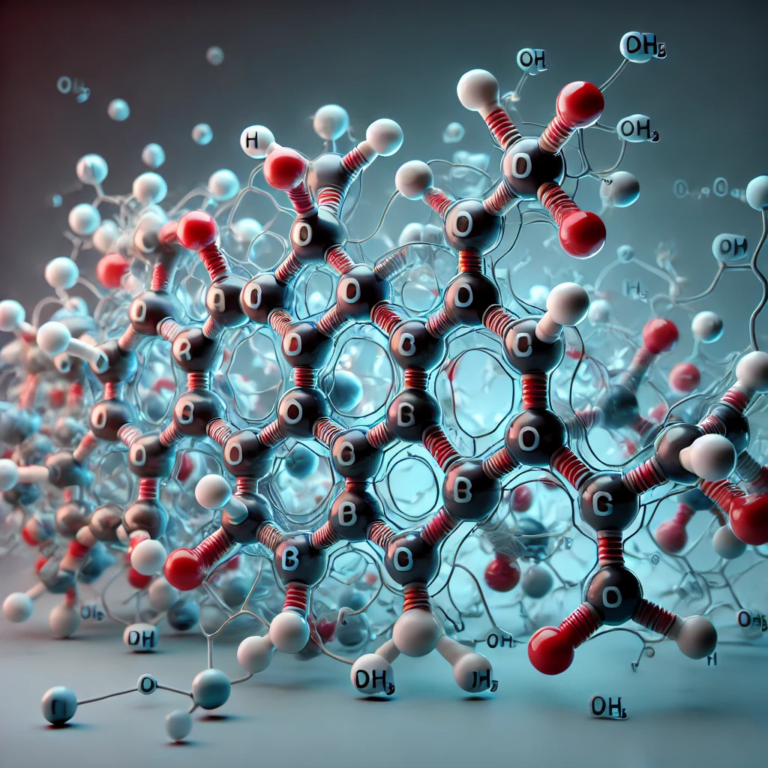
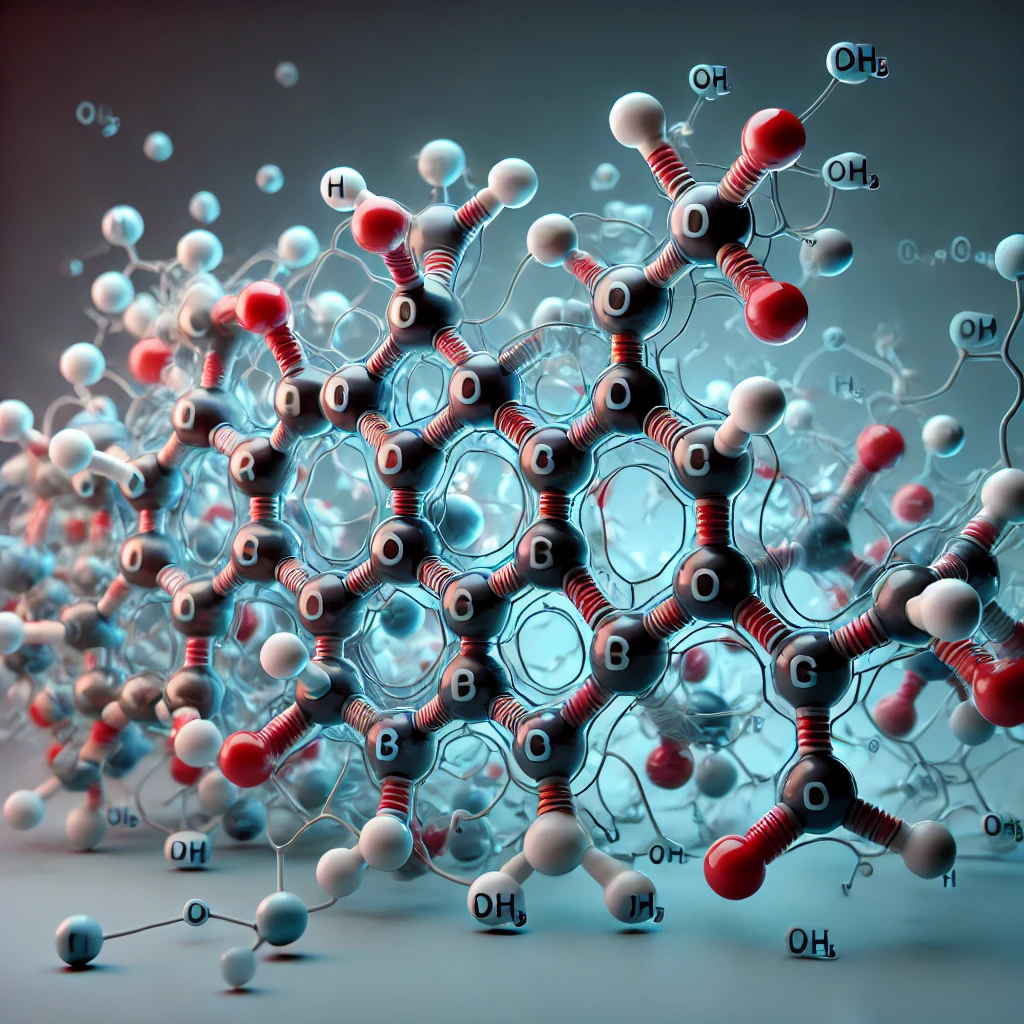
Mechanism of Action of Amphotericin B
The primary Amphotericin B mechanism of action is its ability to bind to ergosterol, a vital component of fungal cell membranes. Once bound, it creates pores in the membrane, leading to leakage of cellular contents and ultimately, cell death. This mechanism is highly effective against fungi but can also affect human cells, which is why careful dosing is essential.
Types of Infections Treated by Amphotericin B
Amphotericin B is versatile in treating various fungal infections:
- Superficial Mycoses: These are fungal infections that affect the skin, nails, and mucous membranes. Amphotericin B can be used topically or systemically to manage these conditions.
- Systemic Mycoses: These are more severe infections that spread throughout the body, often affecting vital organs. Amphotericin B is particularly valuable in treating systemic mycoses like cryptococcosis, histoplasmosis, and aspergillosis, especially in immunocompromised individuals.
Side Effects Amphotericin B
Amphotericin B, while effective against a broad range of fungal infections, is known for its significant side effects. These side effects can be categorized into two main types: infusion-related reactions and cumulative toxicity.
1. Infusion-Related Reactions
These are immediate reactions that occur during or shortly after the administration of Amphotericin B, particularly with the conventional formulation.
- Fever and Chills: These are the most common infusion-related side effects, often referred to as “shake and bake” syndrome. Patients may experience high fever accompanied by severe chills and rigor.
- Nausea and Vomiting: Gastrointestinal discomfort, including nausea and vomiting, is common during infusion. These symptoms can be distressing and may require premedication with antiemetics.
- Headache: Some patients report headaches during or after the infusion of Amphotericin B, which can vary in intensity from mild to severe.
- Hypotension: A drop in blood pressure can occur, leading to symptoms of dizziness, lightheadedness, or fainting. This requires careful monitoring, especially in patients with pre-existing cardiovascular conditions.
- Dyspnea (Shortness of Breath): Difficulty breathing or shortness of breath can occur, especially in patients with pre-existing respiratory issues. This may be a sign of a more severe reaction and requires immediate medical attention.
- Anaphylaxis: Although rare, anaphylactic reactions, which are severe allergic responses, can occur. Symptoms may include difficulty breathing, swelling of the face or throat, rapid heart rate, and a drop in blood pressure.
2. Cumulative Toxicity
These side effects develop over time with continued use of Amphotericin B, especially at higher doses or with prolonged treatment.
- Nephrotoxicity (Kidney Damage): The most serious side effect of Amphotericin B is nephrotoxicity, which can lead to acute kidney injury (AKI). This occurs due to the drug’s tendency to damage the renal tubules, leading to impaired kidney function. Signs of nephrotoxicity include decreased urine output, elevated blood urea nitrogen (BUN), and creatinine levels. Patients on Amphotericin B require regular monitoring of kidney function and adjustments in dosage to minimize damage.
- Electrolyte Imbalances: Amphotericin B can cause significant disturbances in electrolyte levels, particularly potassium (hypokalemia) and magnesium (hypomagnesemia). These imbalances can lead to muscle cramps, weakness, cardiac arrhythmias, and, in severe cases, life-threatening complications. Patients often need supplementation with potassium and magnesium during treatment.
- Anemia: The drug can cause a reduction in red blood cells, leading to anemia. This occurs due to suppression of erythropoietin production.
- Liver Toxicity: Although less common than nephrotoxicity, Amphotericin B can also cause hepatotoxicity, leading to elevated liver enzymes and, in rare cases, liver damage.
- Cardiotoxicity: In some cases, Amphotericin B can lead to cardiac toxicity, manifesting as arrhythmias or other heart-related issues. This is more likely in patients with pre-existing heart conditions or those experiencing significant electrolyte imbalances.
Forms of Amphotericin B
Amphotericin B is available in several formulations, each with different administration requirements and toxicity profiles:
- Conventional Amphotericin B (Deoxycholate Formulation):
The original form of Amphotericin B is dissolved in deoxycholate, a bile salt, to enhance its solubility. This formulation is effective but is also associated with significant toxicity, particularly nephrotoxicity. - Liposomal Amphotericin B (e.g., AmBisome):
Liposomal Amphotericin B is a refined formulation where the drug is encapsulated within liposomes, which are tiny, spherical vesicles made of lipid bilayers. This formulation improves the drug’s delivery to the fungal cells while minimizing its exposure to human tissues, thereby reducing toxicity. This advancement has made treatments like AmBisome more tolerable for patients, especially those who require prolonged therapy. - Amphotericin B Lipid Complex (ABLC):
This formulation combines Amphotericin B with phospholipids, creating a lipid complex that also helps reduce nephrotoxicity while maintaining efficacy. - Amphotericin B Colloidal Dispersion (ABCD):
ABCD involves the combination of Amphotericin B with cholesteryl sulfate, forming a colloidal dispersion that can reduce toxicity compared to the conventional form.
AmBisome: A Key Liposomal Amphotericin B
- What is AmBisome?
AmBisome is a liposomal formulation of Amphotericin B that is designed to improve the safety and efficacy of the drug. The liposomes encapsulate the Amphotericin B, allowing for targeted delivery to infected tissues while reducing the risk of nephrotoxicity, a common side effect of Amphotericin B.
2. Clinical Uses of AmBisome
AmBisome is used to treat a wide range of fungal infections, including those caused by resistant strains. It is particularly beneficial in treating systemic infections and in patients who have a higher risk of side effects from traditional Amphotericin B formulations.
Routes of Administration
Amphotericin B is typically administered intravenously (IV), but the exact route and method depend on the type and severity of the infection:
- Intravenous Infusion (IV):
The most common method of administering Amphotericin B is through slow IV infusion. This method allows the drug to be delivered directly into the bloodstream, ensuring it reaches systemic infections. IV administration is particularly important for treating life-threatening systemic mycoses. - Topical Application:
For superficial mycoses or localized infections, topical Amphotericin B can be applied . This method minimizes systemic absorption and reduces the risk of systemic side effects, making it ideal for treating skin, eye, or mucosal infections. - Intrathecal Administration:
Intrathecal Amphotericin B may be administered (directly into the cerebrospinal fluid) rarely to treat fungal meningitis. This method is used when the infection is resistant to other treatments or when systemic administration is insufficient to reach the central nervous system. - Inhalation:
For pulmonary fungal infections, inhaled Amphotericin B can be used. This method delivers the drug directly to the lungs, targeting respiratory infections while reducing systemic exposure.
Dosage Guidelines
| Formulation | Usual Dosage (mg/kg/day) | Administration Method | Infusion Time |
| Conventional Amphotericin B (Deoxycholate) | 0.5 to 1.5 mg/kg/day | Intravenous (IV) infusion | 4 to 6 hours |
| Liposomal Amphotericin B (AmBisome) | 3 to 5 mg/kg/day (up to 10 mg/kg/day for severe cases) | Intravenous (IV) infusion | Typically 2 hours |
| Amphotericin B Lipid Complex (ABLC) | 5 mg/kg/day | Intravenous (IV) infusion | Approximately 2 hours |
| Amphotericin B Colloidal Dispersion (ABCD) | 3 to 4 mg/kg/day | Intravenous (IV) infusion | 3 to 4 hours |
| Intrathecal Administration | Varies (Consult with specialist) | Directly into cerebrospinal fluid | Specially monitored, varies per case |
| Topical Application | Varies (Consult with specialist) | Direct application to affected area | N/A |
| Inhalation | Varies (Consult with specialist) | Inhaled directly to lungs | N/A |
Note
- Renal Function Monitoring: For all formulations, regular monitoring of kidney function (serum creatinine, BUN) is essential.
- Electrolyte Management: Supplementation of potassium and magnesium may be necessary.
- Premedication: Antipyretics, antihistamines, or corticosteroids may be used to manage infusion-related reactions.
Resistance to Amphotericin B
Fungal resistance to Amphotericin B is relatively rare but can occur, particularly in patients who have received prolonged treatment. Resistance mechanisms may involve alterations in the fungal cell membrane, reducing the drug’s ability to bind to ergosterol. Preventing resistance involves using Amphotericin B judiciously and in combination with other antifungals when necessary.
Recent Advances in Amphotericin B
Recent research has focused on developing new formulations of Amphotericin B that reduce toxicity while maintaining or enhancing efficacy. These advancements include novel lipid-based formulations and the exploration of combination therapies that synergize with Amphotericin B to overcome resistant infections.
Conclusion
Amphotericin B remains a critical drug in the fight against severe fungal infections. Its unique mechanism of action, broad-spectrum efficacy, and the advent of liposomal formulations like AmBisome have ensured its place in modern medicine. However, the drug’s use requires careful management to balance its potent antifungal activity with its potential side effects. As research continues to evolve, Amphotericin B will likely remain at the forefront of antifungal therapy, providing hope for patients with life-threatening infections.
FREQUENTLY ASKED QUESTIONS (FAQ’s)
What is the difference between liposomal and traditional Amphotericin B?
Liposomal Amphotericin B, such as AmBisome, is encapsulated in liposomes to reduce toxicity and improve drug delivery, making it safer than traditional formulations.
How does Amphotericin B treat systemic mycoses?
Amphotericin B binds to ergosterol in fungal cell membranes, causing cell death and effectively treating systemic infections that spread throughout the body.
Which species are most vulnerable to fungal infection?
Species most vulnerable to fungal infections include immunocompromised humans (such as those with HIV/AIDS, cancer patients undergoing chemotherapy, or organ transplant recipients) and animals with weakened immune systems. Additionally, amphibians are highly susceptible to chytridiomycosis, a devastating fungal infection affecting many species worldwide.
Can Amphotericin B be used during pregnancy?
Amphotericin B is generally considered safe during pregnancy, particularly in life-threatening infections, but it should be used under strict medical supervision.

Dr. Hamza is a medical content reviewer with over 12 years of experience in healthcare research and patient education. He specializes in evidence-based health information, medications, and chronic disease management. His reviews are based on trusted medical sources and current clinical guidelines to ensure accuracy, transparency, and reliability. All content reviewed by Dr. Hamza is intended for educational purposes only and should not be considered a substitute for professional medical advice