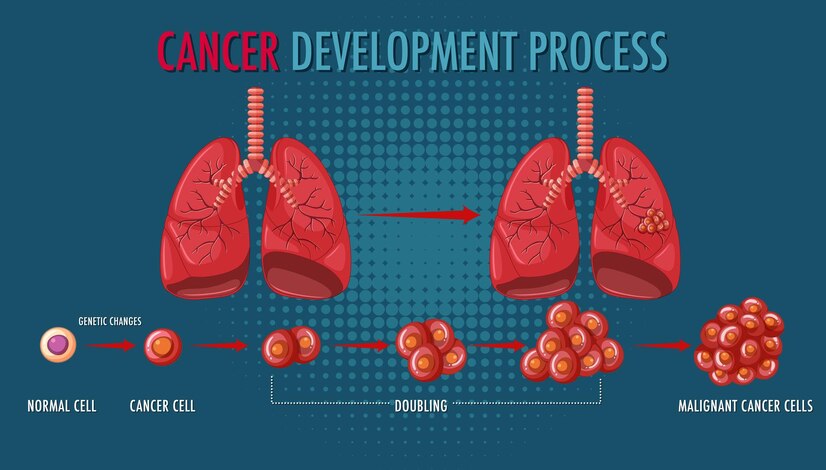
Discover the world of oncologic diseases—what causes cancer, how it spreads, and the latest breakthroughs in treatment. Stay informed, stay ahead!. Oncologic diseases, more commonly known as cancers, are a group of conditions characterized by the uncontrolled growth and division of abnormal cells. These abnormal cells can invade surrounding tissues and organs indeed, spread to distant corridors of the body through a process called metastasis. This uncontrolled growth can disrupt organ function and eventually lead to life-long complications.
Understanding the Fundamentals:
- Cell Growth and Division: Our bodies are made up of trillions of cells, which constantly divide and grow to repair and replace damaged tissues. This process is tightly regulated, ensuring controlled growth and preventing unnecessary cell proliferation.
- Oncogenes and Tumor Suppressor Genes: Genes play a crucial role in regulating cell growth. Mutations in specific genes, known as oncogenes, can promote uncontrolled cell division, while mutations in tumor suppressor genes can hinder the body’s natural checks and balances on cell growth.
- Metastasis: Cancer cells have the ability to invade surrounding tissues and travel through the bloodstream or lymphatic system to establish secondary tumors (metastasis) in distant organs. This is a hallmark of advanced cancer and significantly complicates treatment.
What is the difference between a normal cell and a cancerous cell?
The key differences between normal cells and cancerous cells lie in their growth, behavior, and interaction with the surrounding environment:
Normal cells divide in a controlled manner, following specific signals and stopping when they reach a certain density or maturity. This ensures organized tissue development and repair. While Cancerous cells divide uncontrollably, disregarding the usual signals and density limitations,. This leads to the formation of tumors—masses of abnormal cells.
Types of Oncological Disease
Cancers are broadly classified into five main groups based on the type of cell they originate from:
- Carcinomas: These are the most common type of cancer, accounting for about 80% of all cancers. They arise from epithelial cells, which are the cells that cover the surface of the body and line its organs and glands.
Some common examples of carcinomas include:
- Breast cancer: Cancer that begins in the breast tissue.
- Lung cancer: Cancer that starts in the lungs.
- Colon cancer: Cancer that starts in the colon or rectum.
- Prostate cancer: Cancer that starts in the prostate gland.
- Skin cancer: Cancer that starts in the skin.
2) Sarcomas: These cancers arise from connective tissues, such as bones, muscles, cartilage, fat, blood vessels, and lymph vessels.
Some common examples of sarcomas include:
- Osteosarcoma: Cancer of the bone.
- Liposarcoma: Cancer of fat tissue.
- Leiomyosarcoma: Cancer of smooth muscle tissue.
- Fibrosarcoma: Cancer of fibrous connective tissue.
3) Leukemias: These are cancers of the blood-forming tissues, primarily the bone marrow. They affect the white blood cells, which are essential for fighting infection.
There are four main types of leukemia:
- Acute lymphocytic leukemia (ALL): This is the most common type of leukemia in children.
- Chronic lymphocytic leukemia (CLL): This is a slow-growing type of leukemia that usually affects adults.
- Acute myeloid leukemia (AML): This is a fast-growing type of leukemia that can affect people of all ages.
- Chronic myeloid leukemia (CML): This is a slow-growing type of leukemia that usually affects adults.
4) Lymphomas: These cancers arise from the lymphatic system, which is a network of vessels and tissues that help fight infection.
There are two main types of lymphomas:
- Hodgkin lymphoma: This type of lymphoma is characterized by the presence of Reed-Sternberg cells, a specific type of abnormal cell.
- Non-Hodgkin lymphoma: This is a more common type of lymphoma that includes a variety of subtypes.
5) Myelomas: These are cancers of the plasma cells, which are a type of white blood cell that produces antibodies.
- Myeloma primarily affects the bones, where it can cause bone pain, fractures, and other problems.
Stages of Cancer
Most cancers are assigned a stage based on how advanced they are. This staging system typically uses Roman numerals (I, II, III, IV), with higher numbers indicating a more advanced cancer.
- Stage 0 (Carcinoma in situ): This is a very early stage where abnormal cells are present but haven’t spread beyond their original location. It’s often considered pre-cancerous and has a high cure rate.
- Stage I: The cancer is small and localized, meaning it hasn’t grown into nearby tissues or spread to the lymph nodes.
- Stages II & III: The cancer is larger and may have grown into surrounding tissues. It might also involve lymph nodes near the original site but hasn’t reached distant organs. Stage III can sometimes indicate a larger tumor or more extensive lymph node involvement.
- Stage IV: This is the most advanced stage, where the cancer has metastasized, meaning it has spread to other organs or distant lymph nodes. At this stage, the cancer is generally considered incurable, but treatment can focus on managing the disease and improving quality of life.
Symptoms of cancer
- Unexplained weight loss
- Fatigue
- Pain
- Fever
- Night sweats
- Changes in bowel or bladder habits
- Unusual bleeding or discharge
- Lumps or bumps
- indigestion or trouble swallowing
- Changes in the skin
Causes of cancer
Cancer development is complex and not caused by a single factor. It’s generally a combination of genetic and environmental influences:
- Inherited mutations: Some people inherit changes (mutations) in their genes from a parent that increase their risk of developing cancer. These are less common but can play a role.
- Acquired mutations: Mutations can also happen throughout a person’s life due to errors when cells copy themselves or from exposure to carcinogens.
- Carcinogens: Exposure to certain substances, like tobacco smoke, ultraviolet (UV) radiation, and some chemicals, can damage DNA and lead to cancer.
- Diet and weight: Unhealthy diets high in processed meats, red meat, and low in fruits and vegetables can increase cancer risk. Obesity is also linked to some cancers.
- Infections: Chronic infections with certain viruses, bacteria, or parasites can contribute to cancer development.
- Hormones: Hormone replacement therapy and some hormonal imbalances may increase the risk of certain cancers.
3) Lifestyle factors:
- Tobacco use: Smoking is the single biggest risk factor for cancer. It damages DNA and contributes to various cancers.
- Alcohol consumption: Excessive alcohol consumption can increase the risk of cancers like mouth, throat, liver, and breast cancer.
- Physical inactivity: Regular physical activity can help reduce cancer risk.
- Environmental pollution: Exposure to air, water, or soil pollution can increase cancer risk.
Diagnosis and test
When it comes to diagnosing cancer, there’s no single one-size-fits-all test. Doctors employ a multi-pronged approach, utilizing a combination of procedures and tests depending on the suspected type and location of the cancer.
- Imaging Tests:
- X-rays: These provide basic pictures of bones and sometimes soft tissues, helping detect abnormalities like tumors or masses.
- Computed Tomography (CT) Scans: It generates detailed cross-sectional images of organs, tissues, and bones. They can reveal tumor size, location, and spread to nearby structures.
- Magnetic Resonance Imaging (MRI): MRIs use strong magnets and radio waves to produce detailed images of organs, soft tissues, and bones. They’re particularly useful for differentiating between cancerous and non-cancerous tissues.
- Positron Emission Tomography (PET) Scans: PET scans involve injecting a radioactive tracer that gets absorbed by cells with high metabolic activity, often cancerous tumors. This helps visualize the spread of cancer throughout the body, especially useful for staging (determining advancement). PET scans are often combined with CT scans (PET-CT) for a more comprehensive picture.
2) Biopsies:
- Biopsy is the gold standard for definitively diagnosing cancer. A small tissue sample is extracted from the suspected area, usually with a needle (fine-needle aspiration) or a surgical procedure. The sample is then examined by a pathologist under a microscope to identify cancerous cells.
3) Blood Tests:
- Complete Blood Count (CBC): This basic blood test can reveal abnormalities like anemia, which can sometimes be associated with cancer.
- Tumor Marker Tests: These tests measure the levels of certain substances in the blood that may be elevated in specific cancers. However, they’re not definitive for cancer diagnosis and can be influenced by other factors.
4) Endoscopic Procedures:
- Endoscopes are thin, flexible tubes equipped with a light and camera. They can be inserted through natural openings like the mouth, rectum, or vagina to directly visualize internal organs and potentially take biopsies. Common examples include:
- Colonoscopy: Examines the inner lining of the colon and rectum for polyps or tumors.
- Bronchoscopy: Examines the airways (bronchi) of the lungs for abnormalities.
- Esophagoscopy: Examines the lining of the esophagus (the tube connecting the throat to the stomach) for abnormalities.
5) Other Procedures:
- Bone Marrow Aspiration and Biopsy: Samples of bone marrow are extracted to check for abnormalities in blood cell production, which can be indicative of leukemia or lymphoma.
- Lymph Node Biopsy: Lymph nodes are part of the immune system and can sometimes be the first site where cancer spreads. A lymph node biopsy removes a lymph node for examination to see if cancer cells are present.
Additional Considerations:
- Choosing the most appropriate diagnostic tests depends on individual factors like symptoms, medical history, and suspected cancer type.
- Some tests are minimally invasive, while others may require sedation or anesthesia.
- Doctors will discuss the risks and benefits of each procedure with the patient before proceeding.
- Test results may take time, and often a combination of tests is needed for a definitive diagnosis.
Early detection is crucial for successful cancer treatment. If you experience any concerning symptoms, don’t hesitate to consult a doctor for prompt evaluation.
Management and Treatment
Cancer treatment is no longer a one-size-fits-all approach. Thanks to advancements in medicine, there are a variety of treatment options available, and the best course of action depends on several factors specific to each case.
- Curative Treatments:
These treatments aim to completely eliminate cancer cells and achieve a cure.
- Surgery: This remains a cornerstone of cancer treatment, aiming to remove the cancerous tumor and surrounding tissue with clear margins.
- Radiotherapy: High-energy radiation beams are used to target and destroy cancer cells. Radiation can be delivered externally from a machine or internally (brachytherapy) using radioactive implants placed near the tumor.
- Chemotherapy: Powerfully built drugs are used to kill cancer cells throughout the body. Chemo can be given intravenously, orally, or topically, depending on the specific medication. It’s often administered in cycles with periods of rest for recovery.
2) Adjuvant Therapy:
This type of treatment is given after the primary treatment (surgery, radiation) to eliminate any microscopic cancer cells that may remain and reduce the risk of recurrence. Chemotherapy and radiation are common forms of adjuvant therapy.
3) Palliative Care:
Palliative care focuses on improving a patient’s quality of life by managing symptoms such as pain, fatigue, nausea, and anxiety. It can be provided throughout the course of the illness, alongside curative or other treatments.
4) Emerging Therapies:
- Targeted Therapy: These drugs target specific molecules or pathways involved in cancer cell growth and survival. They offer a more personalized approach with potentially fewer side effects.
- Immunotherapy: This treatment helps the body’s immune system recognize and attack cancer cells. There are different forms of immunotherapy, including immune checkpoint inhibitors and CAR T-cell therapy.
Factors Affecting Treatment Choice
- Type and stage of cancer: The stage (extent of spread) also plays a role in determining the most appropriate approach.
- Patient’s overall health: Age, general health, and presence of other medical conditions are considered to ensure the patient can tolerate treatment.
- Patient’s preferences: Doctors discuss treatment options with the patient, considering their individual preferences and goals of care.
Cancer management and treatment have come a long way, offering a wider range of options with improved effectiveness and reduced side effects. Early detection remains crucial, and if you have any concerns, don’t hesitate to consult a healthcare professional.
